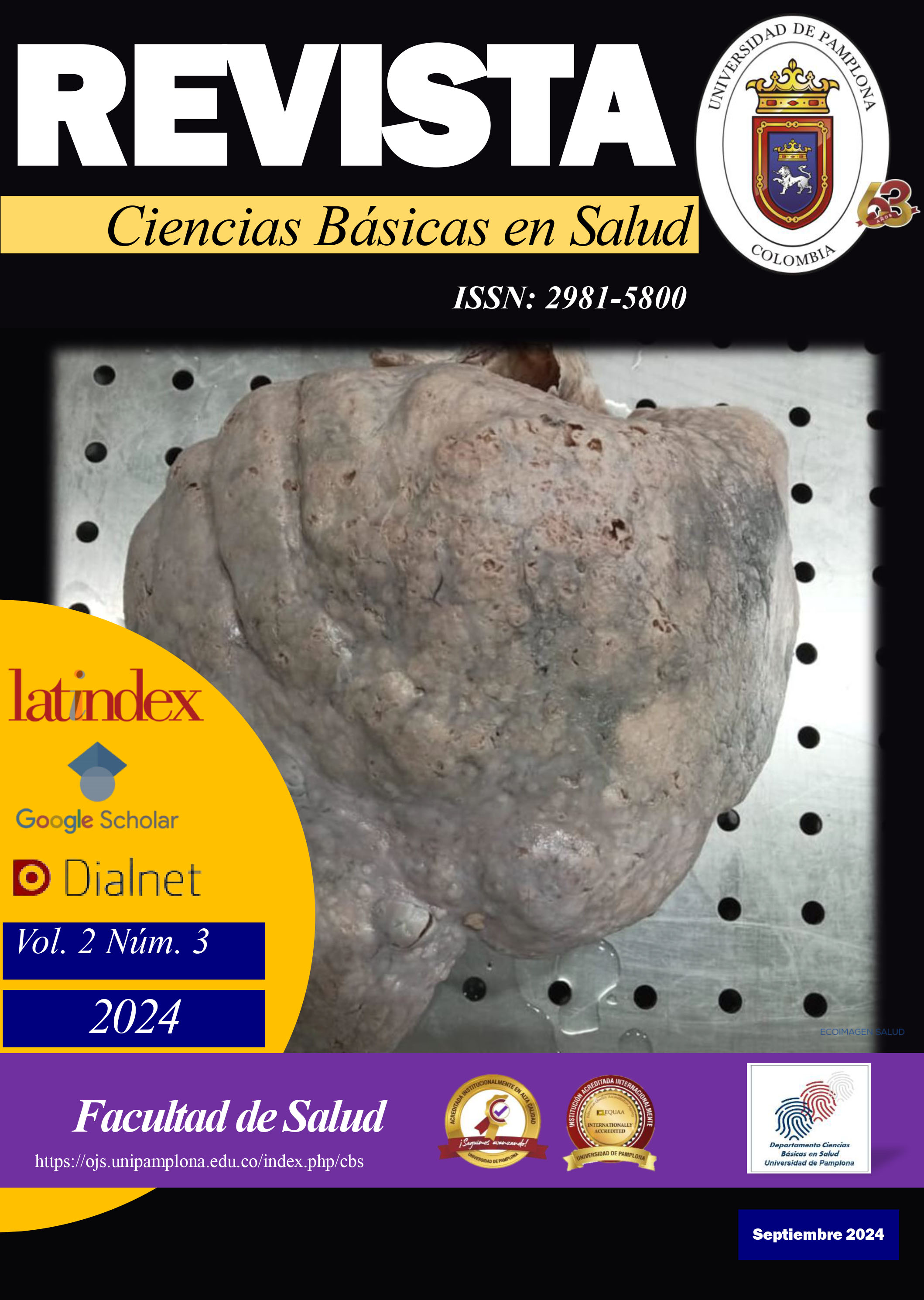
Falla hepática aguda de probable etiología metabólica: Tirosinemia tipo I: Reporte de caso y revisión de la literatura
DOI:
https://doi.org/10.24054/cbs.v2i3.3094Palabras clave:
falla hepática aguda, tirosinemia, trasplante hepáticoResumen
Introducción: La falla hepática aguda es una enfermedad multisistémica infrecuente, pero potencialmente fatal, que se presenta en un niño previamente sano con rápida progresión a la disfunción hepática y falla severa de la síntesis. Las principales causas se pueden agrupar así: infecciosas, metabólicas (tirosinemia, galactosemia), fármacos, vasculares, hepatitis autoinmune, neoplasias e indeterminada. La tirosinemia tipo I (THI) es una enfermedad autosómica recesiva causada por la deficiencia de la enzima fumarilacetoacetato hidrolasa. La THI es una enfermedad rara, se calcula una frecuencia no mayor de 1 caso cada 100.000 recién nacidos vivos en la población mundial. Caso: paciente femenina de 5 años al ingreso con datos clínicos de falla hepática aguda de probable etiología metabólica por reporte de paraclínicos y anatomía patológica se sospechó de una Tirosinemia tipo I. Conclusiones: El tratamiento consiste en la administración de nitisinona y de forma simultánea se debe instaurar una dieta restringida en proteínas. El pronóstico está determinado por el riesgo de carcinoma hepatocelular que aumenta con el retraso del inicio del tratamiento.
Descargas
Referencias
Squires RH, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al. Acute liver failure in children: The first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006 May;148(5):652-658.e2.
Squires JE, McKiernan P, Squires RH. Acute Liver Failure. Clin Liver Dis. 2018 Nov;22(4):773–805.
Chakrapani A, Gissen P, McKiernan P. Disorders of Tyrosine Metabolism. In: Inborn Metabolic Diseases. Berlin, Heidelberg: Springer Berlin Heidelberg; 2016. p. 265–75.
Russo PA, Mitchell GA, Tanguay RM. Tyrosinemia: A Review. Pediatric and Developmental Pathology. 2001 May 10;4(3):212–21.
Jorquera R, Tanguay RM. The Mutagenicity of the Tyrosine Metabolite, Fumarylacetoacetate, Is Enhanced by Glutathione Depletion. Biochem Biophys Res Commun. 1997 Mar;232(1):42–8.
Bliksrud YT, Ellingsen A, Bjoras M. Fumarylacetoacetate inhibits the initial step of the base excision repair pathway: implication for the pathogenesis of tyrosinemia type I. J Inherit Metab Dis. 2013 Sep 9;36(5):773–8.
Endo F, Sun M S. Tyrosinaemia type I and apoptosis of hepatocytes and renal tubular cells. J Inherit Metab Dis. 2002 May;25(3):227–34.
Grompe M, St. Louis M, Demers SI, Al Dhalimy M, Leclerc B, Tanguay RM. A Single Mutation of the Fumarylacetoacetate Hydrolase Gene in French Canadians with Hereditary Tyrosinemia Type I. New England Journal of Medicine. 1994 Aug 11;331(6):353–7.
van Spronsen FJ TYSGLJCPFVBRHH. Hereditary tyrosinemia type I: a new clinical classification with difference in prognosis on dietary treatment. Hepatology. 1994 Nov 20;1187–91.
Forget S, Patriquin HB, Dubois J, Lafortune M, Merouani A, Paradis K, et al. The kidney in children with tyrosinemia: sonographic, CT and biochemical findings. Pediatr Radiol. 1999 Jan 29;29(2):104–8.
Chinsky JM, Singh R, Ficicioglu C, van Karnebeek CDM, Grompe M, Mitchell G, et al. Diagnosis and treatment of tyrosinemia type I: a US and Canadian consensus group review and recommendations. Genetics in Medicine. 2017 Dec;19(12):1380–95.
Ibarra-González I, Ridaura-Sanz C, Fernández-Lainez C, Guillén-López S, Belmont-Martínez L, Vela-Amieva M. Hepatorenal Tyrosinemia in Mexico: A Call to Action. In 2017. p. 147–56.
Baumann U, Preece MA, Green A, Kelly DA, McKiernan PJ. Hyperinsulinism in tyrosinaemia type I. J Inherit Metab Dis. 2005 Apr 13;28(2):131–5.
Morrow G, Tanguay RM. Biochemical and Clinical Aspects of Hereditary Tyrosinemia Type 1. In 2017. p. 9–21.
Morrow G, Angileri F, Tanguay RM. Molecular Aspects of the FAH Mutations Involved in HT1 Disease. In 2017. p. 25–48.
Demers SI, Russo P, Lettre F, Tanguay RM. Frequent mutation reversion inversely correlates with clinical severity in a genetic liver disease, hereditary tyrosinemia. Hum Pathol. 2003 Dec;34(12):1313–20.
Squires RH, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al. Acute liver failure in children: The first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006 May;148(5):652-658.e2.
Squires JE, McKiernan P, Squires RH. Acute Liver Failure. Clin Liver Dis. 2018 Nov;22(4):773–805.
Chakrapani A, Gissen P, McKiernan P. Disorders of Tyrosine Metabolism. In: Inborn Metabolic Diseases. Berlin, Heidelberg: Springer Berlin Heidelberg; 2016. p. 265–75.
Russo PA, Mitchell GA, Tanguay RM. Tyrosinemia: A Review. Pediatric and Developmental Pathology. 2001 May 10;4(3):212–21.
Jorquera R, Tanguay RM. The Mutagenicity of the Tyrosine Metabolite, Fumarylacetoacetate, Is Enhanced by Glutathione Depletion. Biochem Biophys Res Commun. 1997 Mar;232(1):42–8.
Bliksrud YT, Ellingsen A, Bjoras M. Fumarylacetoacetate inhibits the initial step of the base excision repair pathway: implication for the pathogenesis of tyrosinemia type I. J Inherit Metab Dis. 2013 Sep 9;36(5):773–8.
Endo F, Sun M S. Tyrosinaemia type I and apoptosis of hepatocytes and renal tubular cells. J Inherit Metab Dis. 2002 May;25(3):227–34.
Grompe M, St.-Louis M, Demers SI, Al-Dhalimy M, Leclerc B, Tanguay RM. A Single Mutation of the Fumarylacetoacetate Hydrolase Gene in French Canadians with Hereditary Tyrosinemia Type I. New England Journal of Medicine. 1994 Aug 11;331(6):353–7.
van Spronsen FJ TYSGLJCPFVBRHH. Hereditary tyrosinemia type I: a new clinical classification with difference in prognosis on dietary treatment. Hepatology. 1994 Nov 20;1187–91.
Forget S, Patriquin HB, Dubois J, Lafortune M, Merouani A, Paradis K, et al. The kidney in children with tyrosinemia: sonographic, CT and biochemical findings. Pediatr Radiol. 1999 Jan 29;29(2):104–8.
Chinsky JM, Singh R, Ficicioglu C, van Karnebeek CDM, Grompe M, Mitchell G, et al. Diagnosis and treatment of tyrosinemia type I: a US and Canadian consensus group review and recommendations. Genetics in Medicine. 2017 Dec;19(12):1380–95.
Ibarra-González I, Ridaura-Sanz C, Fernández-Lainez C, Guillén-López S, Belmont-Martínez L, Vela-Amieva M. Hepatorenal Tyrosinemia in Mexico: A Call to Action. In 2017. p. 147–56.
Baumann U, Preece MA, Green A, Kelly DA, McKiernan PJ. Hyperinsulinism in tyrosinaemia type I. J Inherit Metab Dis. 2005 Apr 13;28(2):131–5.
Morrow G, Tanguay RM. Biochemical and Clinical Aspects of Hereditary Tyrosinemia Type 1. In 2017. p. 9–21.
Morrow G, Angileri F, Tanguay RM. Molecular Aspects of the FAH Mutations Involved in HT1 Disease. In 2017. p. 25–48.
Demers SI, Russo P, Lettre F, Tanguay RM. Frequent mutation reversion inversely correlates with clinical severity in a genetic liver disease, hereditary tyrosinemia. Hum Pathol. 2003 Dec;34(12):1313–20.
de Laet C, Dionisi-Vici C, Leonard J V, McKiernan P, Mitchell G, Monti L, et al. Recommendations for the management of tyrosinaemia type 1. Orphanet J Rare Dis. 2013 Dec 11;8(1): eight.
Shah I, Shah F. Tyrosinemia type I: Case series with response to treatment to NTBC. Indian Journal of Gastroenterology. 2016 May 25;35(3):229–31.
van Spronsen FJ, van Rijn M, Meyer U, Das AM. Dietary Considerations in Tyrosinemia Type I. In 2017. p. 197–204.
Liu Y, Luo Y, Xia L, Qiu BJ, Zhou T, Feng MX, et al. Living donor liver transplantation for children with tyrosinemia type I. J Dig Dis. 2020 Mar 25;21(3):189–94.
Ascher Bartlett JM, Yanni G, Kwon Y, Emamaullee J. Pediatric acute liver failure: Reexamining key clinical features, current management, and research prospects. Vol. 28, Liver Transplantation. John Wiley and Sons Ltd; 2022. p. 1776–84.
Kawabata K, Kido J, Yoshida T, Matsumoto S, Nakamura K. A case report of two siblings with hypertyrosinemia type 1 presenting with hepatic disease with different onset time and severity. Mol Genet Metab Rep. 2022 Sep; 32:100892.
Geppert J, Stinton C, Freeman K, Fraser H, Clarke A, Johnson S, et al. Evaluation of pre-symptomatic nitisinone treatment on long-term outcomes in Tyrosinemia type 1 patients: a systematic review. Orphanet J Rare Dis. 2017 Dec 11;12(1):154.
Barone H, Bliksrud YT, Elgen IB, Szigetvari PD, Kleppe R, Ghorbani S, et al. Tyrosinemia Type 1 and symptoms of ADHD: Biochemical mechanisms and implications for treatment and prognosis. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2020 Mar 21;183(2):95–105.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Revista Ciencias Básicas en Salud

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.