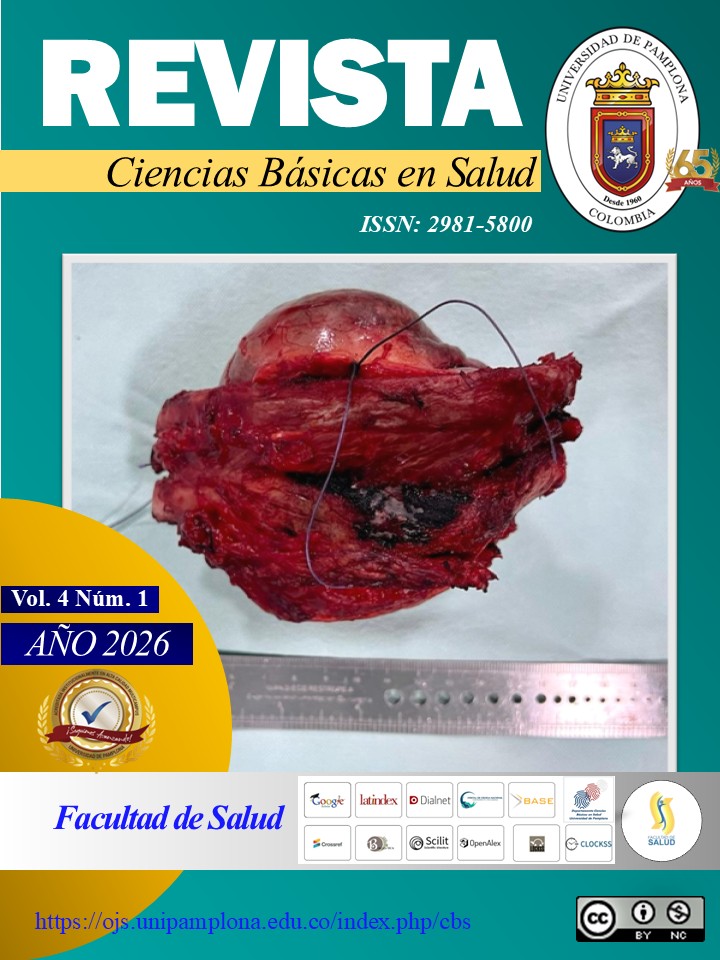
Perineal reconstruction in fournier’s gangrene: the role of the lotus petal flap in the current paradigm
DOI:
https://doi.org/10.24054/cbs.v4i1.4294Keywords:
Fournier’s gangrene, perineal reconstruction, lotus petal flap, fasciocutaneous flaps, abdominoperineal resection, preoperative DopplerAbstract
Introduction. Perineal reconstruction after major pelvic resections and in Fournier’s gangrene requires well-vascularized tissue to obliterate dead space with low donor-site morbidity. The lotus petal flap (LPF)—a fasciocutaneous flap based on internal pudendal perforators—provides close skin concordance in color and thickness and notable technical versatility. Methods. Narrative review of current indications, operative steps, and modifiers of outcomes for the LPF, prioritizing recent clinical series and comparative studies, including variants (bilateral, oversized) and Doppler-guided planning. Results. The LPF is valuable for large defects after APR/ELAPE, complex rectovaginal/rectoperineal fistulas, and vulvar/labial reconstruction. Technique: prone design, ischium–scrotum/vagina–anus triangle, Doppler localization of perforators, and a 3–4 cm base; in extensive defects, combine a deepithelialized petal (volume) with a cutaneous petal (cover). Outcomes are influenced by defect size, surgical timing (delay until a clean bed in infection), and comorbidities (diabetes, prior irradiation). Discussion. Predominantly retrospective evidence supports the LPF when high-quality skin coverage and abdominal wall preservation are prioritized; evidence gaps remain versus muscular flaps for very large pelvic cavities.Conclusion. The LPF should be considered the first-line fasciocutaneous option when reliable coverage and moderate dead-space obliteration are needed; success hinges on precise indication, perforator-based design, and appropriate timing.
Downloads
References
Niranjan NS. Perforator flaps for perineal reconstructions. Semin Plast Surg. 2006;20(2):133–144. doi:10.1055/s-2006-941721.
Papas Y, Laurent R, Efanov IJ, Paek L, Danino MA. Oversized lotus petal flap for reconstruction of extensive perineal defects following abdomino perineal resection. Ann Chir Plast Esthet. 2022;67(4):224–231. doi:10.1016/j.anplas.2022.06.001
Arfaoui R, Ferjaoui MA, Khedhri S, Abdessamia K, Hannechi MA, Neji K. Lotus petal flap for unusual indication: A recto-vaginal fistula with perineal defect after vaginal delivery. Int J Surg Case Rep. 2021;86:106337. doi:10.1016/j.ijscr.2021.106337
Buja Z. Lotus petal flap reconstruction of labia major and perineum after necrotizing fasciitis infection: a case report. SAGE Open Med Case Rep. 2024;12:2050313X241242593. doi:10.1177/2050313X241242593
Hellinga J, Stenekes MW, Werker PMN, Janse M, Fleer J, van Etten B. Quality of life, sexual functioning, and physical functioning following perineal reconstruction with the lotus petal flap. Ann Surg Oncol. 2020;27(13):5279–5285. doi:10.1245/s10434-020-08771-5; Hellinga J, Fleer J, van der Lei B, Werker PMN, van Etten B, Stenekes MW. Aesthetic outcomes of perineal reconstruction with the lotus petal flap. Plast Reconstr Surg Glob Open. 2021;9(6):e3621. doi:10.1097/GOX.0000000000003621)
Eseme EA, Scampa M, Viscardi JA, Ebai M, Kalbermatten DF, Oranges CM. Surgical outcomes of VRAM vs. gracilis flaps in vulvo-perineal reconstruction following oncologic resection: a proportional meta-analysis. Cancers (Basel). 2022;14(17):4300. doi:10.3390/cancers14174300
Galbraith NJ, McCollum C, Di Mascio L, Lowrie J, Hinckley M, Lo S, et al. Effect of differing flap reconstruction strategies in perineal closure following advanced pelvic oncological resection: a retrospective cohort study. Int J Surg. 2023;109(11):3375–3382. doi:10.1097/JS9.0000000000000617
Warrier SK, Kimble FW, Blomfield P. Refinements in the lotus petal flap repair of the vulvo-perineum. ANZ J Surg. 2004;74(8):684-8. doi:10.1111/j.1445-1433.2004.03119.x
Rennert RC, Januszyk M, Sorkin M, Gurtner GC. Lotus petal flaps for perineal reconstruction: a functional and aesthetic assessment. J Plast Reconstr Aesthet Surg. 2013;66(9):1231-6. doi:10.1016/j.bjps.2013.05.015
Khalifian S, Kim J, Bhanot P. Perineal reconstruction with the lotus petal flap: indications, outcomes, and patient satisfaction. Ann Plast Surg. 2014;72(2):188-93. doi:10.1097/SAP.0000000000000037)
Horta R, Silva Á, Carvalho A, Amarante J, Silva P. Reconstruction of complex perineal defects with lotus petal flaps after Fournier gangrene. J Plast Surg Hand Surg. 2016;50(2):120-4. doi:10.3109/2000656X.2015.1110273
Chang CC, Lan YT, Jiang JK, Chang SC, Yang SH, Lin CC, Lin HH, Wang HS, Chen WS, Lin TC, Lin JK. Risk factors for delayed perineal wound healing and its impact on prolonged hospital stay after abdominoperineal resection. World J Surg Oncol. 2019;17(1):226. doi:10.1186/s12957-019-1768-4
Oosta-Hellinga J. Reconstruction using the lotus petal flap: applications and outcomes [dissertation]. Groningen: University of Groningen; 2021. doi:10.33612/diss.174535273.
O Hellinga J, Khoe PC, van Etten B, Hemmer PH, Havenga K, Stenekes MW, Eltahir Y. Fasciocutaneous lotus petal flap for perineal wound reconstruction after extralevator abdominoperineal excision: application for reconstruction of the pelvic floor and creation of a neovagina. Ann Surg Oncol. 2016;23(12):4073-9. doi:10.1245/s10434-016-5332-y.
Bodin F, Dissaux C, Seigle-Murandi F, Dragomir S, Rohr S, Bruant-Rodier C. Posterior perineal reconstructions with "supra-fascial" lotus petal flaps. J Plast Reconstr Aesthet Surg. 2015;68(1):e7–e12. doi:10.1016/j.bjps.2014.10.028) (Hellinga J, Fleer J, van der Lei B, Werker PMN, van Etten B, Stenekes MW. Aesthetic outcomes of perineal reconstruction with the lotus petal flap. Plast Reconstr Surg Glob Open. 2021;9(6):e3621. doi:10.1097/GOX.0000000000003621
Grossi U, Minicozzi A, Vitagliano T, Ruggiero A, Bassi N, Ruffolo C, et al. Bilateral lotus petal flap reconstruction for perianal Paget’s disease. Tech Coloproctol. 2020;24(12):1319-23. doi:10.1007/s10151-020-02283-w.
Woon CY, Chong SJ, Tan BK. Internal pudendal perforator artery flap harvesting without preoperative imaging. J Plast Reconstr Aesthet Surg. 2010;63(7):1098-104. doi:10.1016/j.bjps.2009.04.029.
Hellinga J, Fleer J, van der Lei B, Werker PMN, van Etten B, Stenekes MW. Aesthetic outcomes of perineal reconstruction with the lotus petal flap. Plast Reconstr Surg Glob Open. 2021;9(6):e3621. doi:10.1097/GOX.0000000000003621.
Persichetti P, Cogliandro A, Marangi GF, et al. Reconstruction of perineal defects after abdominoperineal resection: the role of fasciocutaneous flaps. Ann Plast Surg. 2007;59(6):659–664.
Goldie SJ, Figus A, Navsaria H, et al. Comparison of vertical rectus abdominis myocutaneous and gracilis flaps for perineal reconstruction. J Plast Reconstr Aesthet Surg. 2016;69(8):1097–1101. doi:10.1016/j.bjps.2016.05.002.
Reilly DJ, Sham EK, Chee JBL, Chauhan A. A novel application of the lotus petal flap in high-risk perineal urethrostomy: principles and outcomes. Australas J Plast Surg. 2018;1(1):134–138. doi:10.34239/ajops.v1i1.17.
Langston DM, Evans D, Moore S, Shen J, Lee Z, Wingate J, Skokan AJ, Liaw A, Hagedorn JC, Breyer BN, Baradaran N. Functional outcomes of Fournier's gangrene: a multi-institutional experience. Can J Urol. 2023 Apr;30(2):11487-11494. PMID: 37074748.
Bodin F, Dissaux C, Seigle-Murandi F, Dragomir S, Rohr S, Bruant-Rodier C. Posterior perineal reconstructions with “supra-fascial” lotus petal flaps. J Plast Reconstr Aesthet Surg. 2015;68(1):e7–e12. doi:10.1016/j.bjps.2014.10.028.
Warrier SK, Kimble FW, Blomfield P. Refinements in the lotus petal flap repair of the vulvo-perineum. ANZ J Surg. 2004;74(8):684–688. doi:10.1111/j.1445-1433.2004.03119.x.
Hellinga J, Khoe PC, van Etten B, et al. Aesthetic outcomes of perineal reconstruction with the lotus petal flap. Plast Reconstr Surg Glob Open. 2021;9(6):e3621. doi:10.1097/GOX.0000000000003621.
Dölen UC. Flap-based reconstruction for the defects of Fournier’s gangrene. Turk J Plast Surg. 2019;27(2):56–61. doi:10.4103/tjps.tjps_61_18.
Buja Z, Salerno IM, Gentili A, et al. Lotus petal flap reconstruction of labia majora and perineum: case report and review. SAGE Open Med Case Rep. 2024;12:2050313X241242593. doi:10.1177/2050313X241242593.
Downloads
Published
Issue
Section
License
Copyright (c) 2026 Revista Ciencias Básicas en Salud

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.